White Papers
Today’s physicians face some unique challenges. Patients are increasingly seeing reduced engagement from physicians who are often rushed and distracted during visits because of the documentation burden, leading to 71% of surveyed patients feeling “frustrated” with their healthcare experience. And with the added frustrations of stressful platform toggling in the shift to telehealth and reimbursements denied due to inaccurate or insufficient documentation, 64% of U.S. physicians say the pandemic has intensified their sense of burnout.
Using their mobile device, physicians unobtrusively record their visits, streaming their speech to the Nuance AI platform, where it gets translated into a clinical node and goes through a quality review process to ensure accuracy before being entered into the EHR. The physician then simply has to review and sign off on the notes, saving time and reducing physician fatigue and burnout.
Scribe programs started with the idea of reducing the data-entry burden on physicians, but high turnover and lack of industry standards and certification for scribes can lead to inconsistent documentation quality and an additional training burden on the physician.
With pandemic-related stress exacerbated by ever-increasing administrative workloads, physician burnout is at an all-time high. How can healthcare organizations help reduce providers’ feelings of burnout and improve the patient experience?
With the annual revenue loss of one physician vacancy estimated at more than $2 million – and the cost to recruit replacements estimated at $250,000 each – losses of $4.68 billion per year can be attributed to physician burnout.
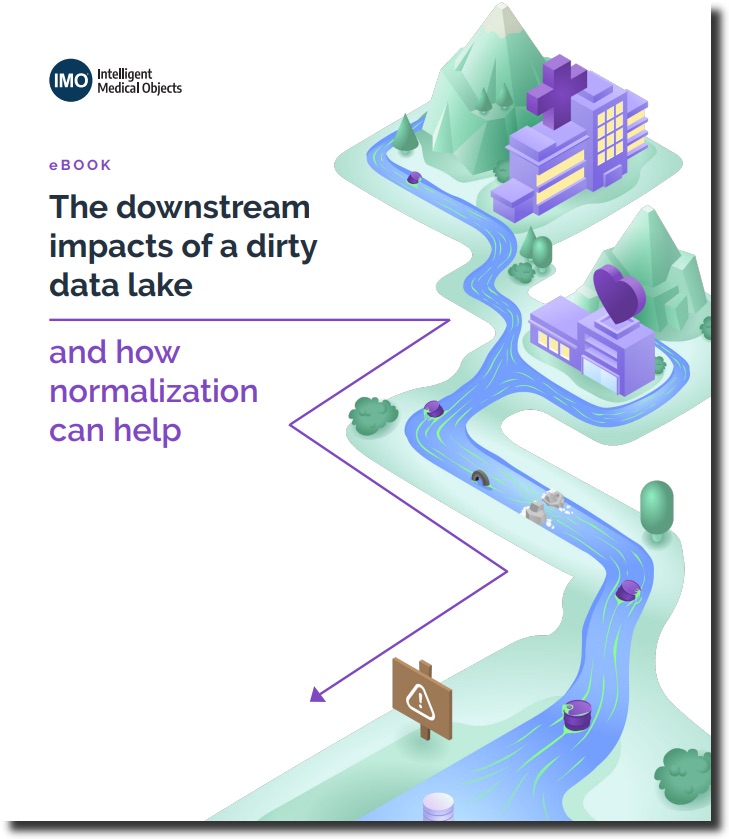
In a recent HIMSS survey, 59% of hospital leadership staff said that they have lost potential reimbursements over the last year due to poor data quality, and 47% reported inaccuracies in their quality reporting due to poor-quality data.
Many EHR problem lists have duplicate entries, outdated diagnoses and other information unrelated to a patient’s present condition, leading to confusion and frustration for clinicians.
Healthcare organizations are facing a crucial deadline to address network and API security requirements tied to the 21st Century Cures Act. Healthcare providers and payers must give patients easier access to their health data and put security in place to guard that data – or face noncompliance penalties.
Healthcare organizations are profitable targets for cybercriminals because of the vast amounts of personal health information (PHI) they store for members. The challenge lies in balancing the need for improving patients’ digital experiences with the importance of having appropriate security measures in place to prevent healthcare fraud and identity theft.
A large health insurance company introduced an innovative Health Rewards program that gamified good health behavior with reward points for gift cards. Unfortunately, the CAPTCHAs added to the site’s login page were no match for automated credential-stuffing cyberattacks that breached thousands of customer accounts and fraudulently redeemed reward points in a gift-card cracking attack.